Have you ever heard of the term ‘fertility window’ and wondered what it means? Or perhaps you’re already familiar with the concept but aren’t quite sure how it applies to your journey towards starting a family? Well, you’re not alone. The fertility window, though a simple concept, is often shrouded in mystery and misconceptions. But understanding this crucial period can be your game-changer when planning a family.
The fertility window refers to the specific days in a woman’s menstrual cycle when pregnancy is possible. It’s like a door that opens up for a limited time each month, presenting the perfect opportunity for sperm to meet egg. This window is typically around 6 days, ending on the day of ovulation. Knowing when this window occurs can significantly increase your chances of conceiving.
But why stop at just knowing your fertility window? Understanding the factors that affect your fertility can provide you with a more comprehensive picture of your reproductive health. Age, for instance, plays a significant role – fertility tends to decrease as we get older. Lifestyle choices such as diet, exercise, and even stress levels can also impact your fertility. And let’s not forget medical conditions, with issues like polycystic ovary syndrome (PCOS) and endometriosis potentially putting a spanner in the works.
Understanding these factors can further empower you and your partner to make informed decisions about your family planning journey. So, are you ready to delve deeper into the fascinating world of fertility windows and take that vital step towards parenthood? Join us as we unravel the mysteries of the fertility window, shedding light on how you can optimize your chances of conceiving. We promise it’s going to be an enlightening ride!
Factors Impacting Fertility
As we embark on the journey of creating life, it’s crucial to understand the landscape that lies ahead. Fertility, or our ability to conceive and bear children, is a complex process influenced by numerous factors. Among these, age and certain medical conditions take center stage.
The Role of Age in Fertility
Time waits for no one, and this holds true for our fertility as well. As we age, both men and women experience a natural decline in their reproductive capabilities. For women, this decline becomes more noticeable in the mid-30s and accelerates after 40. Men, on the other hand, see a more gradual decrease, with notable changes starting around the age of 50. These age-related shifts in fertility are supported by numerous studies and statistics, painting a clear picture of how our biological clock ticks.
While this information might seem daunting, it’s important to remember that every individual is unique. Age is just one piece of the puzzle, and many people successfully conceive and have healthy babies later in life.
Medical Conditions and Fertility – The Need for Awareness
When it comes to fertility, knowledge truly is power. Recognizing the signs of potential fertility issues and seeking medical advice early can make all the difference. There are several medical conditions that can affect fertility, with polycystic ovary syndrome (PCOS) and endometriosis being among the most common.
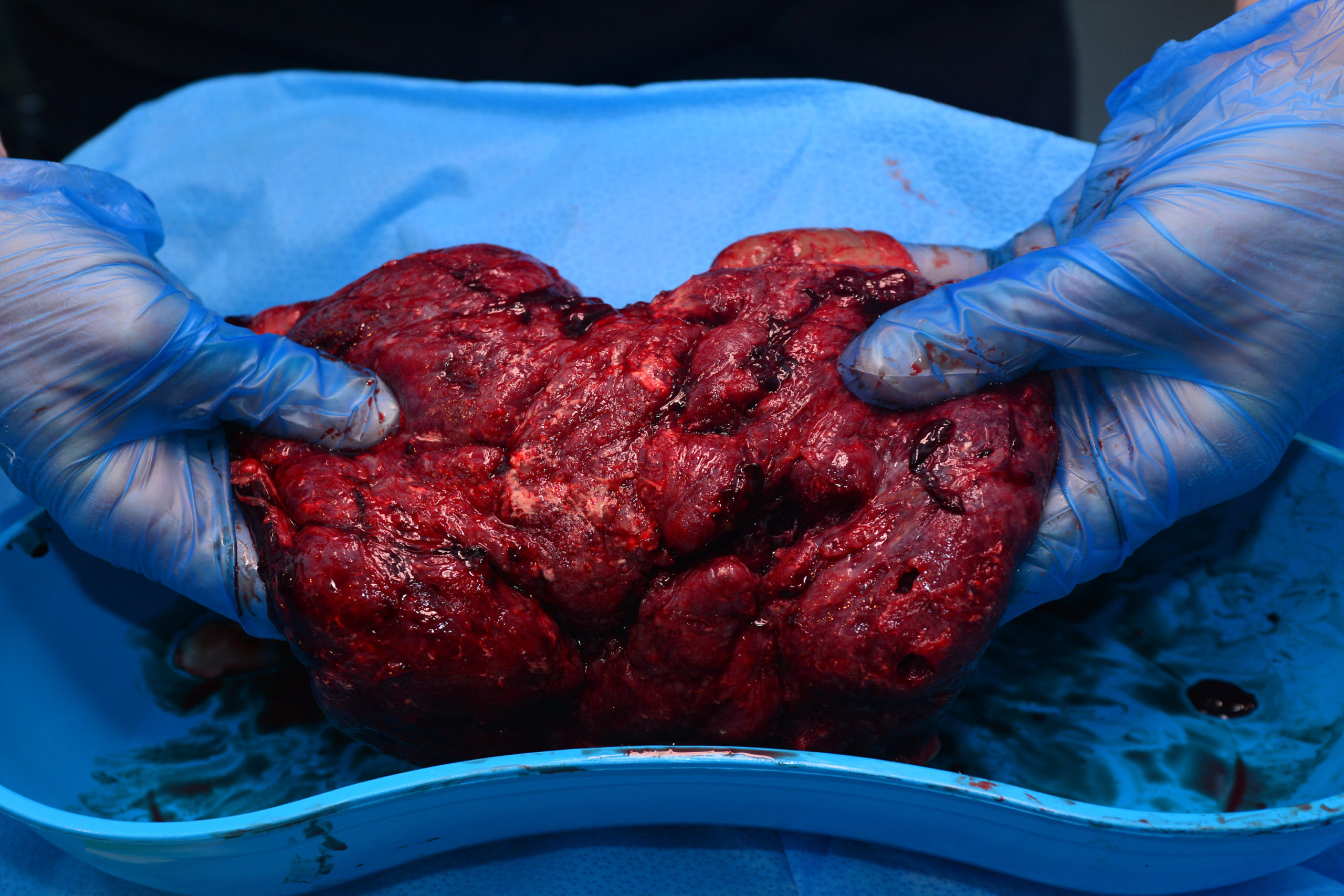
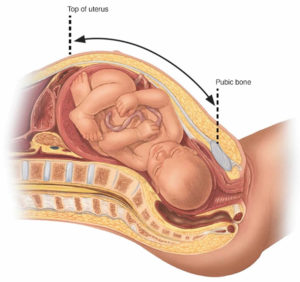
PCOS, a hormonal disorder, can disrupt ovulation and lead to irregular periods, making conception a challenge. Endometriosis, on the other hand, involves the growth of uterine-like tissue outside the uterus, which can cause inflammation and scar tissue, potentially impacting fertility.
Both of these conditions come with their own set of symptoms and potential treatments. It’s crucial to seek medical advice if you suspect you may be affected, as early diagnosis and treatment can significantly improve your chances of conceiving.
Navigating the path to parenthood can sometimes feel like a rollercoaster ride, filled with highs, lows and unexpected turns. But by understanding the factors that influence our fertility, we can better prepare for the journey ahead. Remember, it’s okay to ask for help. Medical professionals are there to guide and support you, every step of the way.
Optimizing Fertility
Healthy Lifestyle
When it comes to fertility, lifestyle choices play a significant role. The journey towards parenthood is not just about the right timing or medical intervention; it’s also about nurturing our bodies and creating the optimal environment for conception.
Maintaining a healthy weight is one of the most critical factors in this process. According to the National Heart, Lung, and Blood Institute, reaching and maintaining a healthy weight can prevent and control many diseases and conditions. When your weight is in a healthy range, your body can more efficiently circulate blood and manage fluid levels, both essential for reproductive health.
Eating a balanced diet is another key element. Proper nutrition provides our bodies with the necessary fuel and nutrients needed for all bodily functions, including reproduction. Incorporating a variety of fruits, vegetables, lean proteins, and whole grains into your diet can significantly improve your fertility.
Regular exercise, too, plays an integral role in fertility. Physical activity helps maintain a healthy weight, regulates hormonal balance, and improves overall well-being, all of which are beneficial for fertility.
Let’s not forget the importance of reducing alcohol consumption and quitting smoking. Both habits can negatively impact fertility, and making the decision to cut back on alcohol and quit smoking can have a significant positive effect on your journey towards parenthood.
Antioxidant Supplements
Antioxidants are like the superheroes of our bodies. They combat oxidative stress, a condition that can damage our cells, including egg and sperm cells. Research has shown that antioxidants can improve fertility in both men and women.
Specific antioxidants, like vitamin C, vitamin E, and coenzyme Q10, have been linked to improved fertility. Vitamin C and E help protect the cells in our bodies from damage, while coenzyme Q10 plays a vital role in energy production, crucial for the function of egg cells.
However, before you rush to the nearest pharmacy to stock up on these supplements, remember: every individual is unique. What works for one person may not work for another. It’s always best to consult with a healthcare professional before starting any new supplements. They can provide personalized advice based on your specific needs and circumstances.
In the end, optimizing fertility is a holistic process. It’s about making conscious choices that benefit not only our reproductive health but our overall well-being. By understanding the importance of a healthy lifestyle and the potential benefits of antioxidant supplements, you’re already one step closer to your journey towards parenthood.
Identifying the Fertile Window
Understanding your body’s fertility signals can be both empowering and instrumental in your journey towards parenthood. The concept of the ‘fertility window’—a crucial period in your menstrual cycle when pregnancy is possible—can provide valuable insights for those trying to conceive. In this post, we’ll explore the physical signs that indicate ovulation and discuss tools that can help you identify this pivotal window of opportunity.
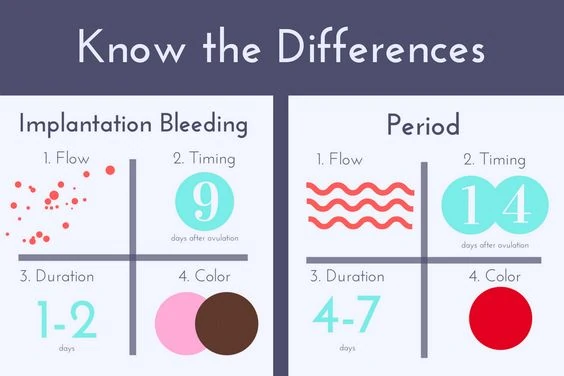
One of the most telling signs of ovulation is a change in your cervical mucus. As you approach ovulation, your body produces more estrogen, causing your cervical mucus to become clear and stretchy, much like raw egg whites. This fertile-quality mucus indicates that you’re in or near your fertility window.
Another sign to watch out for is a slight rise in your basal body temperature (BBT). After ovulation occurs, progesterone levels increase, causing a tiny but detectable rise in your BBT. By tracking these temperature shifts over several cycles, you can start to predict when ovulation typically occurs.
But how exactly do you track these signs? Simple and effective tools are at your disposal. Ovulation predictor kits (OPKs), for instance, measure the level of luteinizing hormone (LH) in your urine. An LH surge usually precedes ovulation by 24 to 36 hours, giving you a heads-up that your fertility window is opening.
On the other hand, fertility apps can offer a digital solution to tracking your menstrual cycle and symptoms. These apps use algorithms to predict your fertility window based on the data you input, such as your period start date, BBT, and cervical mucus changes.
While these methods can be incredibly helpful, remember that each person’s body is unique. Factors such as stress, illness, or disruptions in your normal routine can affect ovulation timing. So, it’s essential to listen to your body and seek professional advice if you have any concerns.
Embarking on your fertility journey can feel like navigating uncharted territory. But understanding your fertility window and recognizing the signs of ovulation can equip you with the knowledge to map your path. Remember, every step you take brings you closer to your dream of parenthood. Here’s to celebrating the power of your body and the miracle of life!
Medical Options for Couples Facing Infertility
There are several medical options available for couples facing infertility:
- In-vitro Fertilization (IVF): This procedure involves fertilizing an egg with sperm outside the body in a laboratory. The fertilized egg (embryo) is then placed in the woman’s uterus.
- Intrauterine Insemination (IUI): This treatment involves placing sperm directly into a woman’s uterus when she is ovulating.
- Fertility Drugs: These medications regulate or induce ovulation, increasing the chances of conception.
- Surgery: For conditions such as endometriosis or blocked fallopian tubes, surgery could improve fertility.
- Assisted Reproductive Technology (ART): Techniques such as surrogacy or egg, sperm, or embryo donation fall under this category.
Key Indicators to Seek Medical Help
Here are some situations where it might be advisable to seek medical help:
- Age: Women over 35 who have been trying to conceive for six months or more.
- Reproductive Health History: Previous miscarriages, irregular menstrual cycles, or known fertility impairments.
- Duration of Trying: If you’ve been having regular unprotected sex for a year (or six months if you’re over 35) without success.
- Underlying Health Conditions: Conditions such as PCOS, endometriosis, or problems with sperm production or function.
Supporting Each Other Through the Process
The journey through fertility treatments can be challenging emotionally and physically. Here are some strategies to support each other:
- Open Communication: Share your feelings honestly and listen to your partner’s concerns.
- Manage Stress: Seek out stress relief techniques such as yoga, meditation, or counseling.
- Stay Positive: Try to maintain a positive outlook and remember that many couples experience similar struggles.
- Seek Support: Join support groups or forums where you can connect with other couples undergoing similar experiences.
Lastly, seeking help from a reproductive endocrinologist—a doctor who specializes in managing infertility—can be beneficial. They can provide you with personalized advice and treatment options based on your specific circumstances. You can find local fertility specialists or online resources through platforms like the American Society for Reproductive Medicine or Resolve: The National Infertility Association.
Remember, every couple’s fertility journey is unique, and there’s no one-size-fits-all approach. Stay informed, seek professional guidance when needed, and support each other every step of the way.
Deciphering Fertility: Your Questions Answered
Embarking on a journey to parenthood can trigger a flurry of questions, especially around fertility and ovulation. As a fertility counselor, I’m here to provide answers to the most asked questions and guide you through understanding your body’s unique fertility signals.
When am I most fertile? How to calculate your ovulation cycle
Your most fertile period, also known as your ‘fertile window,’ typically occurs 6 days ending on the day of ovulation. Ovulation usually happens about 14 days before the start of your next menstrual cycle.
When are you more likely to conceive?
You’re most likely to conceive during your fertile window. This is when an egg is released from your ovaries (ovulation) and sperm has the chance to fertilize the egg.
What is an ovulation calculator and how does it help you get pregnant?
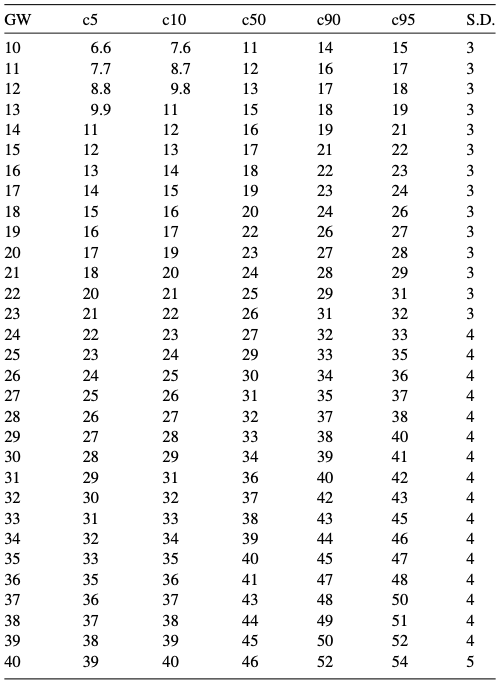
An ovulation calculator provides an estimate of when you’re likely to ovulate based on the date of your last menstrual cycle and the average number of days between your cycles.
Understanding Your Menstrual Cycle
A typical menstrual cycle lasts between 21 to 35 days, with day 1 being the first day of your period. Ovulation, the release of an egg from the ovaries, generally occurs around the middle of your cycle.
When Is the Best Time to Have Baby-Making Sex?
The best time to have sex for conception is during your fertile window, ideally a day or two before ovulation.
How can I spot the signs of ovulation?
Signs of ovulation include changes in cervical mucus (it becomes clear and stretchy), a slight rise in basal body temperature, and mild pelvic pain on one side.
What is Basal body temperature method?
This involves tracking your body’s resting (basal) temperature to identify your fertile window. A slight rise in basal body temperature typically occurs after ovulation due to increased progesterone levels.
How many days after your period can you get pregnant?
This depends on the length of your menstrual cycle and when you ovulate. However, if you have a regular 28-day cycle, you could potentially become pregnant as early as day 11 of your cycle.
When am I ovulating?
In a regular 28-day cycle, ovulation typically occurs around day 14.
What if I have irregular periods?
Irregular periods can make it more challenging to predict ovulation. Seeking advice from a healthcare professional can help you understand your cycle better.
What are Cervical mucus changes?
As you approach ovulation, your cervical mucus becomes clear and stretchy, similar to raw egg whites. This is a sign that you’re in or near your fertility window.
Should I have sex before, during or after ovulation?
To increase your chances of conception, it’s best to have sex in the days leading up to, and including the day of, ovulation.
Using ovulation test kits (also known as ovulation predictor kits)
Ovulation test kits detect the surge in luteinizing hormone (LH) in your urine, which typically occurs 24-36 hours before ovulation.
How else can I prepare for pregnancy?
Maintaining a healthy lifestyle, including a balanced diet, regular exercise, and avoiding harmful substances like alcohol and tobacco, can boost your fertility.
When does preconception health begin?
Preconception health should ideally begin at least three months before you start trying to conceive. It involves taking steps to ensure your body is ready for pregnancy, such as taking folic acid supplements, ensuring a healthy weight, and getting any chronic medical conditions under control.
Final message
As we conclude our enlightening journey through the world of fertility awareness, it’s clear to see that knowledge is indeed power. Understanding your fertility window is not just a tool for conception, but a pathway to deeper self-knowledge and proactive health management.
Throughout this post, we’ve highlighted the importance of being attuned to your body’s rhythms and patterns. We’ve delved into how factors such as age and certain medical conditions can affect fertility, and underscored the value of seeking professional guidance when necessary. Remember, you’re not alone in this journey. Healthcare professionals are there to provide advice, support, and help you navigate any challenges that may arise.
Taking charge of your fertility journey is about more than just planning for a family – it’s about making informed decisions that can contribute to a healthier, happier life. So don’t wait. Be proactive, seek advice, and take the reins on your reproductive health. After all, your fertility journey is a significant part of your life story, and you have the power to write it in a way that aligns with your dreams and aspirations.
So here’s our final call-to-action: Embrace the journey, arm yourself with knowledge, and step confidently into the world of fertility awareness. It’s time to take charge, make informed decisions, and pave the path towards a fulfilling future. You’ve got this!